This is the final part of a series on Mumia Abu-Jamal’s fight for appropriate health care for himself and for over 2 million prison inmates across the country. (Click here for Part I, here for Part II, or here for Part IIIa)
In Abu-Jamal’s case, most of the legal and media discussion has focused on the denial of hepatitis treatment to him and inmates across the country. And while that alone is malpractice, what is even more appalling was the failure to diagnose and then treat his diabetes. Diabetes care is a cornerstone of basic healthcare. Abu-Jamal’s case illustrates that inmates are denied not only expensive medical treatments but also widely available, inexpensive treatments. Moreover, it demonstrates a failure of correctional healthcare systems to provide even the most basic health care for its patients.
Abu-Jamal, nearly a year ago tested positive for diabetes while imprisoned, and yet his case was intentionally left untreated. In his medical records, blood tests taken on March 8, 2015 showed a glucose level of 419, well exceeding the diabetic level of 200.
There are two major forms of Diabetes. Type 1 Diabetes is the kind that frequently presents young in life. While it is very common for this form of diabetes to be initially diagnosed in a crisis setting (coma, severe dehydration, electrolyte disturbances), Type 2 Diabetes, the form that typically starts in adulthood and the form that Abu-Jamal has, very rarely gets to that point because it develops more slowly and is discovered early before it ever reaches that level of severity.
In his chart, someone circled the blood sugar value and wrote by it “on steroids.” What this note suggests is that the provider felt that since there was an explanation for his high blood sugar, there was no need to treat it. That lack of action is equivalent to looking at a patient whose pneumonia is so severe that they need a breathing machine and then saying, “We know why they’re not breathing well. They have pneumonia.” Just because you know the cause of a finding doesn’t mean it doesn’t have to be treated.
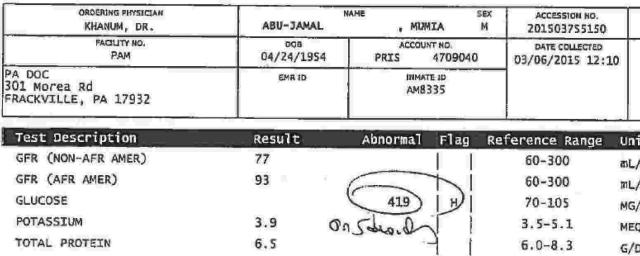 Lab results from Abu-Jamal's medical record
Lab results from Abu-Jamal's medical record
Standard of care for a blood sugar that high is to immediately give medication to lower it, or at least monitor three times a day. One of the main medications for the treatment of diabetes is metformin. It costs $4 a month. But because prison doctors didn’t provide any treatment, his sugars climbed to levels so toxic that his brain stopped functioning and he went into a diabetic coma.
Countrywide epidemic of neglectful healthcare
Sadly, Abu-Jamal’s healthcare is not an exception. It’s an example of the poor healthcare that is rampant in prisons and jails across the country. Cases of this felonious level of healthcare are so numerous that it would be impossible to list them in their entirety. However a few examples illustrate the severity of the negligence.
 Anthony Carvajal had bone cancerAnthony Carvajal, a Florida inmate, needed treatment for cancer, but instead was given ibuprofen for six months. An inmate in California was denied cardiac medications after being discharged from the hospital for heart failure. Ieasha Meyers, an inmate in Iowa, was forced to give birth without medical personnel on the floor of her cell when her reports of contractions went ignored.
Anthony Carvajal had bone cancerAnthony Carvajal, a Florida inmate, needed treatment for cancer, but instead was given ibuprofen for six months. An inmate in California was denied cardiac medications after being discharged from the hospital for heart failure. Ieasha Meyers, an inmate in Iowa, was forced to give birth without medical personnel on the floor of her cell when her reports of contractions went ignored.
The situation in jails is even more deplorable. Because jails, typically run by municipalities or counties, are seen as temporary holding institutions, the quality of healthcare falls short of even that provided by prisons. The justification for this is that the average length of stay in jails is less than 30 days so only minimal healthcare services are needed. However, because of prison over-crowding, inmates, who in many cases are awaiting trial and who may not even be guilty of whatever charge was brought against them, can reside there much longer. Dr. Smith (named changed out of fear of retaliation) is a physician who worked for Advanced Correctional Health Care, a private company that provided services for a network of jails. According to her experience, she saw inmates that were there for over 7 months on a regular basis.
Dr. Smith recalls struggling daily to provide basic the medical care that she knew the inmates deserved. Whether she was requesting a procedure as simple as a dental extraction, attempting to secure a needed medication, or trying to order indicated blood tests, she always came up against the same mantra, “The bottom line of what they said is that you just want to keep people alive. You don’t actually need to treat anything unless to prevent a deterioration of their health.”
The facilities and lack of access horrified her. She provided care for four different jails and opportunities for inmates to see her were extremely limited. She would provide access to patients for 1 or 2 hours once or twice a week at most at each location. Given that most patient visits last 15-20 minutes, at maximum she would see only 8 patients a day. One facility only had her come once every two weeks. Inmates were required to request appointments, and if there wasn’t enough space, they just didn’t get to see the doctor.
Dr. Smith recalls a case where she was called in the middle of the night for a medical emergency. A woman who was 8 months pregnant was being held for failure to appear in court for a minor offense. While locked up she developed acute abdominal pain that Dr. Smith realized required hospital care to treat. She was worried the condition could be fatal to both the inmate and her fetus.
By the time the guards had called Dr. Smith the woman had already been suffering for four hours and her pain was getting worse. When this doctor asked why it had taken the guards so long to contact her, they responded that they thought that the inmate was “just whining.” Though Dr. Smith insisted that they call an ambulance immediately, as precious time had already elapsed, it took them several more hours to transport the patient because they required that she first complete all the paperwork to be “released on her own recognizance.” According to Dr. Smith, this was routine. By doing this, the medical bills would be charged to the patient rather than the jail.
Unfortunately, Advanced Correctional Health Care is no different than most of the other companies in this industry. The four largest companies in corrections healthcare are Corizon Healthcare, Correct Care Solutions, MHM Correctional Services, and Wexford Health Services. Together, the top four companies are responsible for the healthcare of nearly half of the incarcerated population in the United States. Just as in prisons, the examples and lawsuits over egregiously poor healthcare in jails are too numerous to catalog in their entirety, but a few examples demonstrate the atrocities.
 Bradley Ballard and his motherIn Alabama, Tanish Jefferson died from something as simple as constipation. New York City recently terminated their contract with Corizon due to at least two cases where the company’s employees contributed to the deaths of inmates. Bradley Ballard, an inmate at Rikers Island, died after being denied insulin, food, and running water for nearly a week. Correct Care Solutions has been sued for allowing Farah Saleh Farah to die from dehydration in a Virginia jail. In New York, Rashad McNulty died in Westchester County Jail after his complaints of chest pain were ignored. He was having a fatal heart attack. In North Carolina, Jen McCormack also died from a heart attack that was ignored while in jail custody. The list goes on and on.
Bradley Ballard and his motherIn Alabama, Tanish Jefferson died from something as simple as constipation. New York City recently terminated their contract with Corizon due to at least two cases where the company’s employees contributed to the deaths of inmates. Bradley Ballard, an inmate at Rikers Island, died after being denied insulin, food, and running water for nearly a week. Correct Care Solutions has been sued for allowing Farah Saleh Farah to die from dehydration in a Virginia jail. In New York, Rashad McNulty died in Westchester County Jail after his complaints of chest pain were ignored. He was having a fatal heart attack. In North Carolina, Jen McCormack also died from a heart attack that was ignored while in jail custody. The list goes on and on.
All of these companies are for-profit organizations. The motivation of greed over human life is illustrated in not only the poor medical care, but also the poor ethics at the core of these companies.
The president of Correctional Medical Associates, a subsidiary of Corizon, was indicted for embezzlement when he was a medical student. In Alabama, Corizon employed two physicians who had previously lost their licenses for sexual misconduct with patients. Nurses in a California prison are continually so short staffed that in April they threatened to go on strike. The Department of Investigation in New York found 658 fingerprint cards, accumulated over 4 years, that had never processed as part of Corizon’s employee background checks. These self-serving, immoral practices are clearly incompatible with providing healthcare, an industry focused solely on the welfare of patients.
Sustainable change requires a systematic intervention
What’s shocking is that these companies continue to operate despite consistent malpractice. The lack of regulatory oversight of healthcare in correctional facilities is appalling.
Private companies have exploited the poor regulatory standards. There has been a growing trend for correctional facilities to outsource their healthcare. Typically these contracts are negotiated on a per inmate fee. This creates a perverse incentive where the less the healthcare companies spend on each inmate’s health, the more profit they make.
The privatization of healthcare in correctional facilities has been fingered as the root cause of poor healthcare for the over 2 million inmates in US jails and prisons. It is true that greedy business practices that value money over human life is the most direct causal agent to these atrocious conditions. However, they are only exploiting the various city, county, state and federal governments that don’t care enough to require standards to begin with.
Individual whistle blowing, institution-level inquiries, and journalism have identified this criminally poor healthcare for years and yet these poor conditions persist. Interventions on an individual level do not create sustained change. What’s needed is a systems-level approach.
For example, if every department of corrections in the country required accreditation within the first six months of every contract, conditions would improve. In a recent review it was found that “there is considerable evidence…that accreditation programs improve clinical outcomes.”
Money is what really influences behavior, even in the most benevolent of companies. Tying payment to health outcomes guarantees that standards will be met, a fact so obvious that mainstream healthcare systems have been moving in this direction for years. Insurance companies such as Medicare will only pay for services at facilities that meet certain standards, usually indicated by an accreditation from a recognized organization such as The Joint Commission.
Another possibility would be to create a more robust quality tracking system that is tied to payment. For example, one could create a contract that required meeting certain quality metrics. Failure to do so would result in fines or payment withheld. Metrics could range from service indicators such as the time delay between when a patient requests an appointment and is actually seen, to clinical indicators such as how frequently cholesterol is being checked. This is already becoming the standard in the mainstream healthcare system.
It’s possible that linking payment to quality will save the system so much money in litigation and preventable healthcare complications that correctional facilities will suffer no additional cost burden. But it’s also possible that our correctional healthcare budgets are simply too small and that providing humane healthcare will require more money. If that’s the case, as citizens who support a system of involuntary confinement, the responsibility rests on our shoulders.
The majority of inmates are not psychopathic serial killers, but actually people not all that different than those of us outside of bars. They just can’t afford to pay their speeding tickets on time so they’re sent to jail; they just don’t have a solid network of financially stable friends and family that can help them weather tough financial times so they steal things; they may be addicts, but that is increasingly being recognized as an illness, not a crime, or they just don’t have any educational or career opportunities so they join gangs.
This is our system. We punish people who were born with the cards stacked against them. Then, on top of that, when we have them locked up and completely at the mercy of the penal system, we refuse to provide them with basic healthcare, which then only makes it more difficult for them, if they survive incarceration, to create fulfilling, productive lives when they are released.
It’s convenient to blame profit-driven corporations for the poor state of healthcare in prisons and jails so we point our fingers and play the blame game. It’s much harder to realize that we all are also culpable.